The usual caveats apply here. Everything we know about SARS-CoV-2, the virus that causes COVID-19 is new. We’ve only known about it for about 4 months or 5 months. Our understanding is changing daily as researchers around the world mobilize to develop better treatments and vaccines. Research released in this kind of time-frame has, by definition not undergone rigorous scientific review so it too may change as additional data comes in. All that said, a paper by Ni et al. is being submitted for publication that looks at whether SARS-CoV-2 generates lasting immunity by way of antibodies and does that immunity act to neutralize SARS-CoV-2.
First some basics about the human immune response. If this is old hat to you then skip ahead a couple paragraphs. When a pathogen like COVID-19 enters our body, specialized white blood cells like neutrophils and macrophages hunt these pathogens down and directly kill them. The goal of this more primitive evolutionary immune strategy is to try to quickly neutralize pathogens while while buying time for more sophisticated immunity to develop. This innate immune response, in addition to just killing, triggers what is called adaptive immunity, a more recent evolutionary development.
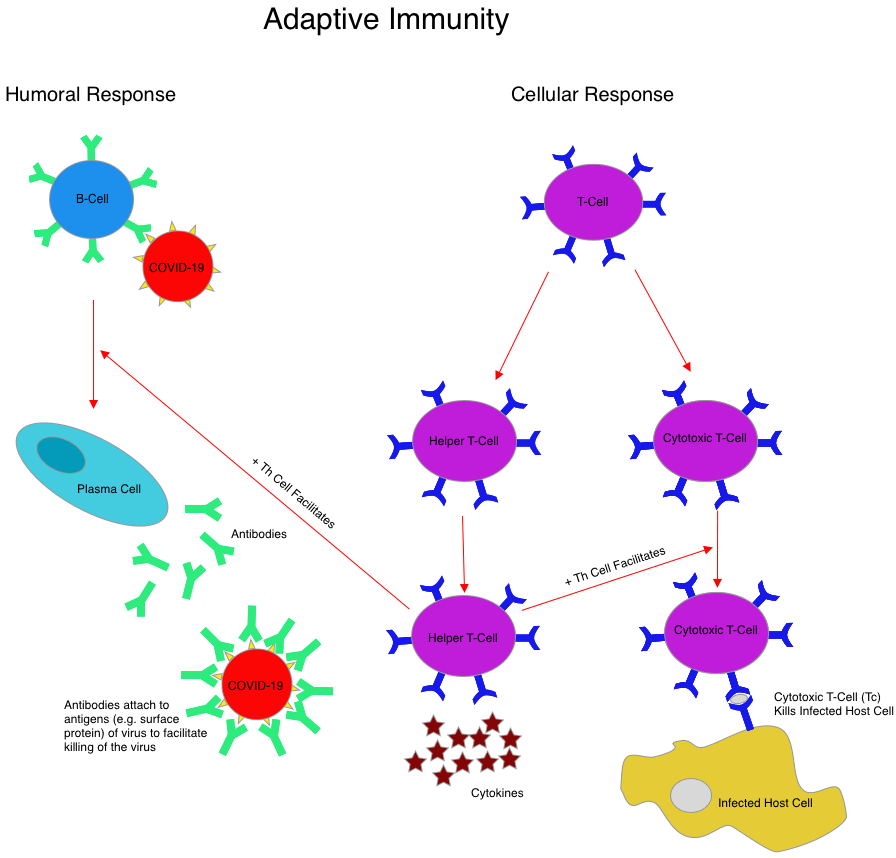
Adaptive immunity involves B-cells (humoral response) and T-cells (cellular response). These cells are attracted to the battle between the specialized white blood cells and the pathogen by signals from the innate immune system cells. B-cells, after coming in contact with a pathogen make antibodies specific to it. These circulating antibodies can then coat the pathogen, making it harder for it to attach to our cells and easier to be identified for killing by other immune cells. Two types of T-cells are important in the immune response to infection. Cytotoxic T-cells become potent killers of cells that have been infected with the pathogen. This is important because an infected cell becomes a factory for making new virus so the body must destroy it to stop the spread. T-helper cells create chemical messages (cytokines) that stimulate the B-cells to make more antibodies to the pathogen, help Cytotoxic T-cells to destroy more infected cells and macrophages to attack the pathogen directly.
Ni et al. looked at 14 patients recovering from COVID-19, 8 on discharge and 6 two weeks after discharge. They found that antibodies to specific antigens (e.g. spike protein on the surface of SARS-CoV-2) were present in both groups of patients after infection. They then looked to see if these antibodies could neutralize SARS-CoV-2. The investigators utilized a pseudovirus particle-based neutralization assay to study the antibody response. This test uses a hybrid virus with components of the pathogen making up the surface but a more harmless retrovirus at its core. This is a useful approach when the virus being studied is particularly dangerous like with SARS-CoV-2 and Ebola and could infect the researchers. With the assay, they showed neutralizing activity from antibodies to the S-RBD (spike protein antigen), indicating that antibodies produced during the immune response can work to neutralize SARS-CoV-2. Finally, they looked at the cellular immune response (T-cell response) to the virus. They isolated monocytes from patients who had been infected and treated them with two important SARS-CoV-2 surface antigens and found that there was an increase in IFN-γ-secreting T cells in recovered patients. This indicates that antigen specific T-cells are produced after infection with SARS-CoV-2. Altogether it appears from this study that both the humoral and cellular immune response have been activated and are working together to create immunity.
So what does all this mean? From this data we can see evidence that the two arms of our immune system are both activated in response to SARS-CoV-2 and that they work together to create immunity that looks like it has all the hallmarks of being sustained. In other words, once infected, it appears that the infected individual should retain some level of immunity to the virus for a prolonged period of time. Here’s hoping!
One reply on “We All Deserve Some Good News on COVID-19”
[…] two anti-viral medications, lopinavir-ritonavir and ribavirin. Interferon beta-1b is part of the innate immune response and it’s utility as an anti-viral has been studied before including during MERS-CoV when it […]
LikeLike