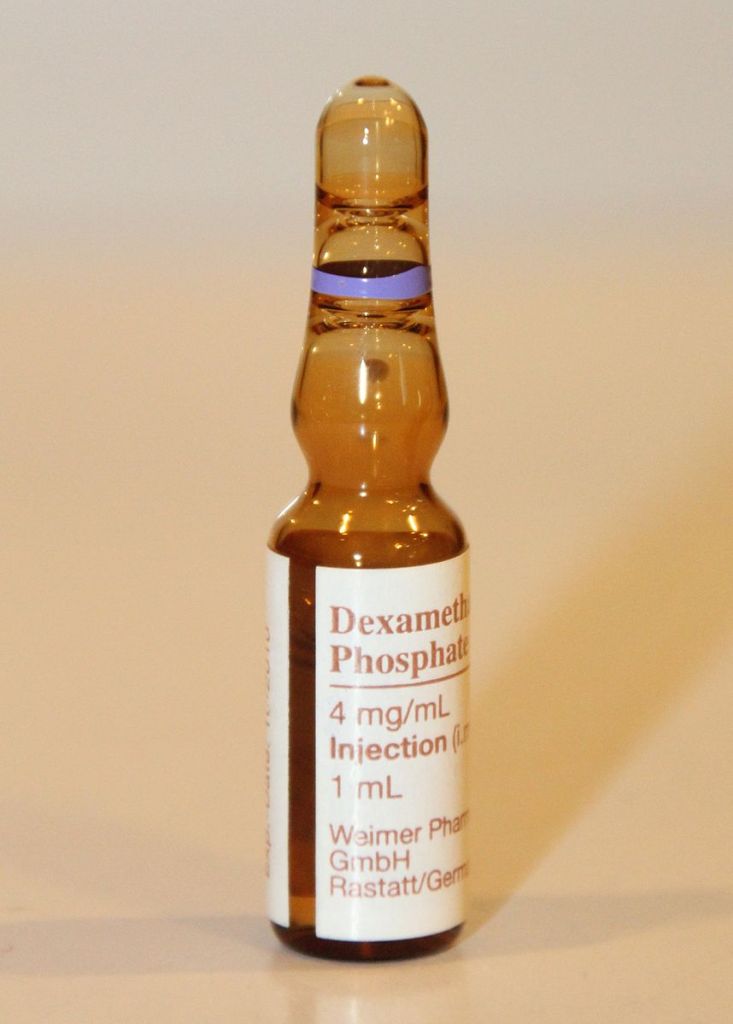
A brief note today on some big COVID-19 news. Researchers from Oxford have announced that they plan to publish very exciting results from a large trial examining potential treatments for COVID-19. They have shown that dexamethasone (Decadron) reduced mortality by one third (28% vs 40%) when given to patients requiring ventilatory support and by 20% (20% vs 25%) for slightly less severe patients who require only oxygen for support. The study included over 2000 patients receiving dexamethasone and compared them to over 4000 patients recieving standard care. It’s likely that the benefit of dexamethasone comes from reducing the body’s inflammatory overreaction to the virus that affects some people with COVID-19 and can lead to multi-organ failure and death. It did not benefit less severe patients, those who don’t require help with breathing, and in those cases giving dexamethasone may prolong the period of viral shedding. So please don’t rush out and put yourself on dexamethasone as many did with hydroxychloroquine. As always, we’d do better if we listened to experts rather than assume knowledge we don’t have because we saw something on the internet.
This is an incredibly important result for a couple of reasons. First, it’s the only drug to date to demonstrate that it saves lives. Remdesivir if you recall, shortens hospital stays and hastens recovery but the data did not reveal that it reduced mortality. Second, dexamethasone is a cheap steroid well known in the medical community to reduce inflammation. The cost of treating someone for 10 days with dexamethasone and saving their life could be as little as $50.
Dropping mortality from 40% to 28% doesn’t sound remarkable but given the scope of this infection and the number of deaths it translates into very tangible improvements in outcome. In the UK for instance, where this study is based, had the medication been given to patients from the start of the pandemic it would have saved 5000 lives.