- Just how many Americans have been exposed to COVID-19 is a difficult number to know with absolute certainty but each day we get closer and closer as serological (antibodies to the virus present in the blood) studies begin to roll in. Many Americans drastically overestimate this number, perhaps as some form of wishful thinking. Current best estimates from ongoing serological studies from the CDC and others puts the positivity rate somewhere around 10% or less nationwide with some regions higher and some lower based on regional disease prevalence to date. Current deaths due to COVID-19 stand at just over 214,000. To obtain herd immunity for COVID-19 we need to reach, at a minimum, 70% of Americans infected. With 214,000 deaths after the first 10% of Americans infected we could expect another one million deaths or more before herd immunity would have any significant protective effect. Even if our ability to treat patients improves enough over time to cut the death rate in half we’d see an additional half a million deaths from a do-nothing approach to the pandemic.
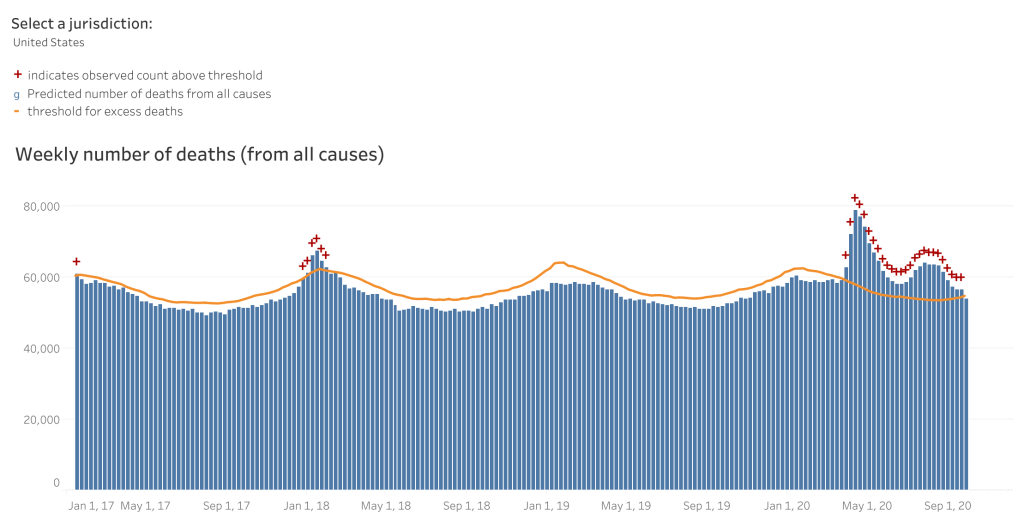
- COVID-19 denialists hold that deaths due to COVID-19 are over-counted. A few weeks ago they gleefully pointed to a CDC report which revealed that 94% of reported deaths were in people with other health issues. To them, this apparently indicated that only 6% of people had actually died from COVID-19. I’m not going to address the fallacy of that thinking here other than to say that if I have diabetes and while crossing the road I get struck by a bus and die, my cause of death is blunt force trauma–pure and simple. We can’t say that diabetes killed me in this case even if my diabetes made my treatment more difficult and played some role in my demise. Diabetes may very well be listed on my death report; I still died from blunt force trauma. The clearest evidence that denialists are wrong here comes from an examination of excess deaths. Epidemiologist can easily examine the previous five or ten years of deaths to establish a predicted number of deaths for the current year. In 2020, as of mid-September, there were 278,000 excess deaths compared with previous years. At that time (September 19, 2020) there were 199,000 deaths attributed to COVID-19. There are two important points here that invalidate the unscientific thinking of COVID-19 denialists in several ways. First, an accounting of excess deaths isn’t an examination of cause of death. It’s simply this: let’s count deaths from the last few years and then let’s count deaths from this year. Guess what, the number this year is bigger…by quite a bit. Where did all those excess deaths come from? It didn’t come from the soul-crushing inability to go to the gym or a favorite nail salon; it came from people dying after being infected with a novel coronavirus. The second important point form this data is that the evidence points to the fact that we’re undercounting COVID-19 deaths. As of September, there have been 278,000 excess deaths but only 199,000 (currently 214,000) deaths reported as due to COVID-19. That means there are nearly 80,000 extra deaths this year that very likely the majority of those were uncounted COVID-19 deaths.
- A report from the CDC shows that Arizona’s institution of mandatory masks significantly reduced transmission of COVID-19 within 2 weeks. A combination of mask mandates and other mitigation strategies (prohibiting large gatherings, temporary closure of bars, gyms and theaters and a reduction in restaurant capacity led to a 75% decline in COVID-19 transmission statewide.
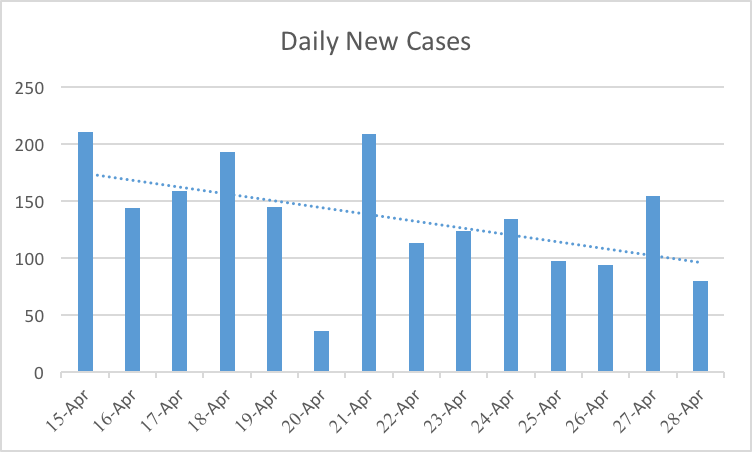
The number of COVID-19 cases stabilized and began to decrease approximately 2 weeks after local officials began mandating mask wearing (throughout several counties and cities) and enhanced sanitation practices
https://www.cdc.gov/mmwr/volumes/69/wr/mm6940e3.htm?s_cid=mm6940e3_w
- A massive study out of India looking at COVID-19 transmission dynamics is well worth reading. I’m going to focus on two important points from the study in part because of their timeliness. First, the study showed that not all spreaders are equal. Approximately 70% of infected individuals did not demonstrate spread to other contacts. Instead, 8% of positive index cases were responsible for nearly two thirds of contact cases. This supports the growing evidence that super-spreading events such as the White House Rose Garden SCOTUS event play an extremely import role in disease spread and underscores the importance of social distancing, mask wear and restricting large groups. The second point I want to highlight from the Indian study shows that children spread the virus at similar rates as seen in adults. The study was unable to examine spread from children to adults but it did show that infected children spread the disease to 18% of their peers. This of course has significant implications for the reopening of schools across the country. As I’ve stated before, to safely reopen schools disease prevalence in the overall community must be very low and testing must be widespread with quick results to allow for rapid isolation of positives and contacts and comprehensive contact tracing. This kind of low community rate comes from grown-ups strictly adhering to non-pharmaceutical interventions such as but not limited to full adherence to mask-wearing and the avoidance of congregating in group settings.