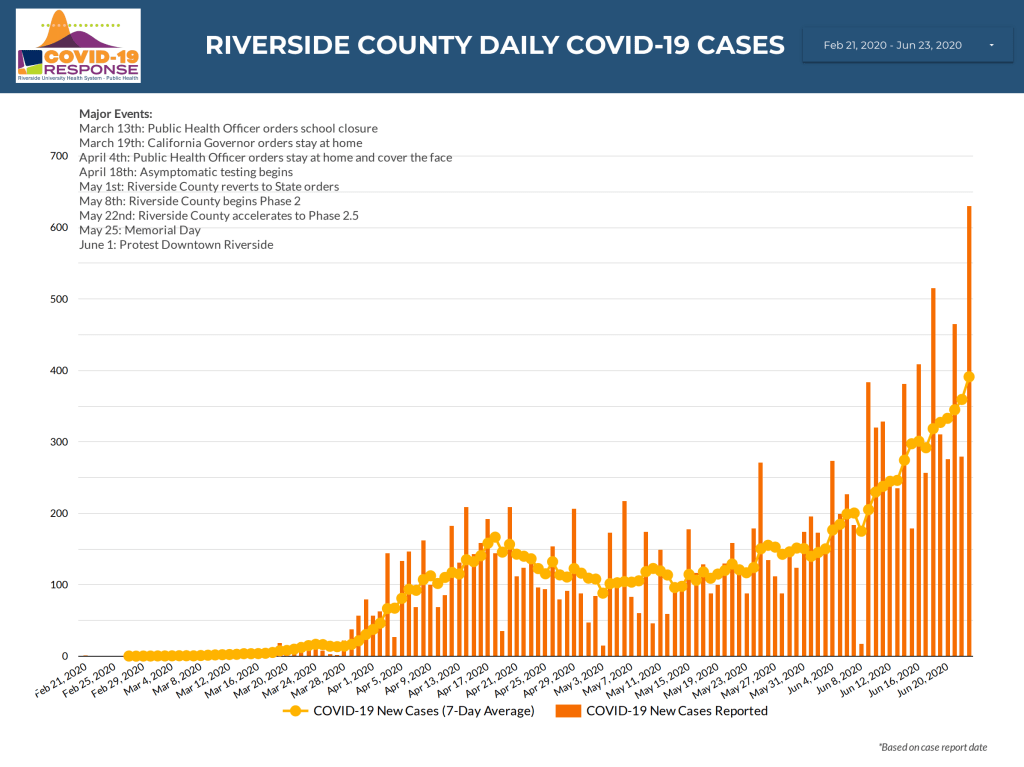
A look today at how we’re doing with COVID-19. First let’s look at my home region, Riverside County. Like much of the country Riverside is seeing significant increases in new daily cases. Over the last week or so we’ve been seeing over 500 new cases each day on most days. Yesterday, Riverside saw its highest daily increase yet with 631 new cases in 24 hours. That compares to fewer than 100 cases per day on most days in mid-April after the initial surge and when social distancing orders were in place. Other metrics are moving in the wrong direction as well: hospitalizations and ICU admits are up but still manageable, the percent-positive rate is up, and doubling-time (time it takes for cases to double) is down. The doubling time maxed out at around 33 days in Riverside a few weeks ago but has now slipped to around 28 days. This is perhaps the most worrisome signal that we’re losing control of the virus in this region. If this trend continues we’ll edge closer and closer to the risk of exponential growth we faced at the beginning of the pandemic. A discussion of exponential growth is beyond the scope of today’s post but at the bottom I’ll post a video of an excellent and understandable explanation of exponential growth and why it isn’t intuitive for most people. The percent-positive rate (rate at which Riverside County’s COVID-19 tests are coming back positive) is at 10%. This is up from a low of around 5 in early May. What this indicates is that our increase in cases is not merely due to increased testing as some political leaders suggest but in fact a true representation of increased prevalence of the virus in the community. Hospitalization rates are an important factor to watch. Daily new cases can be affected by testing rate and the reporting of daily new cases often lags behind as reporting may be slower from sone agencies. Rising hospitalizations show in real-time how a region is doing because it’s a measure of how many people are quite sick, now. Keep an eye on hospitalizations. More people don’t get sick enough to be hospitalized because we test more, more people get really sick because there’s more infection out there.

What about the rest of the country? We’re seeing increasing cases in a number of hotspots around the country. The New York Times tracks where the virus is increasing and we’re seeing significant increases in several hotspots around the country.
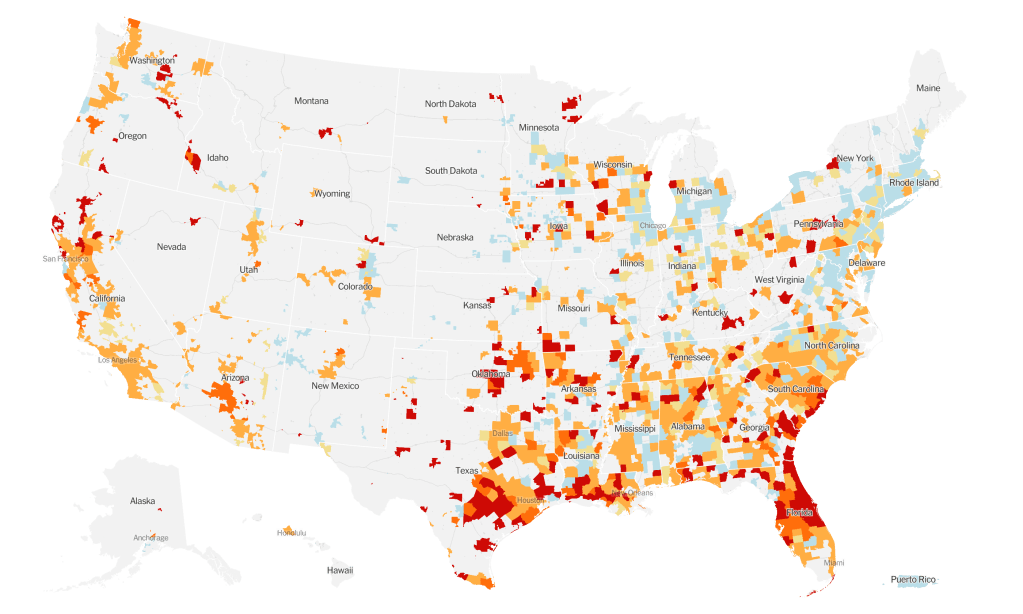
The South was the first region to begin reopening after stay-at-home orders and they’re now the region with some of the most noticeable growth in the last two weeks with 10 states in the region on an increasing trajectory including Texas, Florida, Georgia, North Carolina, Louisiana, Tennessee, Alabama, South Carolina, Mississippi, Arkansas and Oklahoma. Overall, the most concerning regions in the country right now are Florida (reopening began May 4), Arizona (reopening began May 8), Texas (reopening began April 30) and Oklahoma (reopening began April 24). Florida had an 86% increase in new cases over one week and a doubling of their percent-positive rate to 11% in recent days. According to the Sun Sentinel, 75% of adult ICU beds in South Florida are now occupied. The state has had to walk back some of its reopening to address the rising cases there. Arizona has seen their percent-positive rate leap to 20% with an increase in new cases of 90% in a one week period. Oklahoma saw the biggest one week increase with a jump of 111% in new cases. Texas has seen similar increases in percent-positive rate (now at 10%) and new cases (up 86% in a week). More worrisomely, Texas has seen a 60% increase in new hospitalizations. NPR reports that Texas Children’s Hospital in Houston is now admitting adults with COVID-19 to help with the surge, this in spite of the fact that Houston is home to Texas Medical Center, the largest hospital in the world. The growth of the virus in Texas has led some regions within the state to begin mandating facial coverings and Governor Greg Abbot to implore the state’s residents to do so to help keep business open.
“Wearing a mask will help us to keep Texas open.”
Texas Governor Greg Abbott
States that reopened early are not the only states of concern right now and certainly other factors contribute to surges in a region like the recent protests and outbreaks at inpatient institutions. But there are some simple facts that seem to be lost on a significant percentage of Americans: SARS-CoV-2 is here, it’s a dangerous virus that can spread exponentially through an almost completely vulnerable population and no amount of hiding our collective heads in the sand about these previous two facts is going to make it go away. Perhaps the simplest and most effective thing Americans could do to prevent the spread would be to wear a mask when in indoor public spaces and outdoors when social distancing isn’t possible. If the majority of Americans wore a face covering under these circumstances, the spread of SARS-CoV-2 would be significantly limited and businesses would be much less at risk of new closures. As I discussed in a previous post, wearing a mask isn’t for your own protection. The science on masks shows us that if the majority of a population wears face coverings, we, the wearers, spread the virus to fewer people. Wearing a mask protects your neighbor, particularly the most vulnerable, it isn’t to protect you. Your neighbor wears a mask to protect you. If more of us do it, we protect more people. So let’s be neighborly and wear a mask to keep the economy open by stopping the exponential spread of COVID-19, which is starting to happen…again.
Here’s the video that nicely and understandably explains the math of exponential growth.