On March 23, former CDC Director Dr. Tom Frieden published an opinion piece on Fox News suggesting that Vitamin D could be protective against COVID-19. I’ve read the piece and it’s reasonable. Dr. Frieden gave a measured suggestion that maintaining normal Vitamin D levels could help stave off severe illness from COVID-19, particularly in vulnerable populations. He suggested taking a supplement but not overdosing and to check for drug interactions before doing anything. He was clear in stating that we don’t know if this will actually help prevent severe COVID-19 disease but we do know that Vitamin D deficiency is, irrespective of COVID-19, not a good thing.
Right now, we don’t know if Vitamin D deficiency plays any role in the severity of COVID-19. But given the high prevalence of Vitamin D deficiency in this country, it is safe to recommend that people get the proper daily dosage of Vitamin D.
Dr. Tom Frieden/Fox News
I don’t think it was Dr. Frieden’s intention, but from there things have gotten a bit more frenzied. There are a cacophony of voices now screaming the praises of a new cure-all for COVID-19 in the form of Vitamin D and perhaps more worrisomely, a segment of the community opposed to stay-at-home orders using Vitamin D’s possible association with COVID-19 severity as justification for defying this important public health intervention.
This is a bit of complex topic to discuss but I’m going to do my best to talk about the science of Vitamin D as it relates to disease and in particular respiratory diseases like COVID-19.
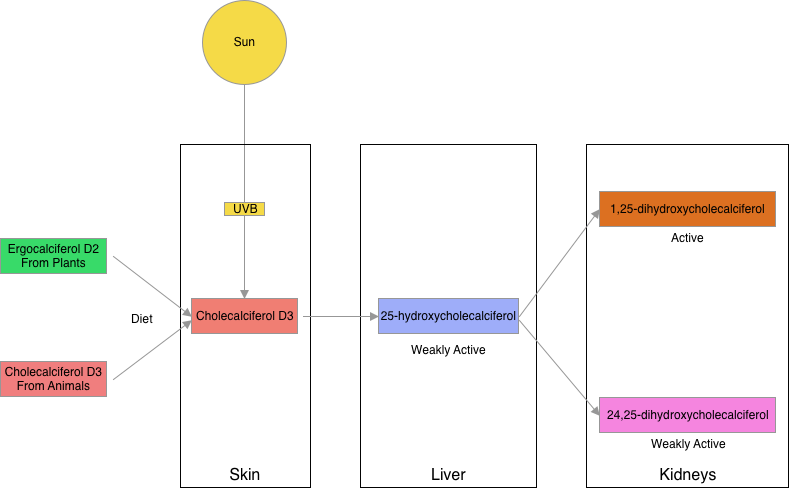
First, and briefly, let’s talk about what Vitamin D is. The term Vitamin D actually describes a group of chemicals important for normal human health. The Vitamin D chemicals are steroid molecules predominantly thought of as an important factor in calcium and phosphorus metabolism in the body and normal bone growth. Many cell types in the body, however, have Vitamin D receptors so its role throughout the body may be more complex and not yet fully understood. Humans get their Vitamin D from a few different sources; one important way to get Vitamin D is to eat it. Ergocalciferol (Vitamin D2) comes from some plants like mushrooms and is the primary form of Vitamin D in fortified foods like milk. Cholecalciferol or Vitamin D3 is found in meat, egg yolks, liver and fatty fish. Humans can also make Vitamin D through sun exposure. A common form of cholesterol (7-dehydrocholesterol) present in skin is converted to cholecalciferol or Vitamin D3–the UV light actually provides the energy for this conversion. So while we can get Vitamin D2 and Vitamin D3 in our diets and through UV light we can make Vitamin D3 in our skin, neither molecule is biologically active for humans. These forms of Vitamin D need to be further converted to active molecules in the liver and then in the kidneys. First, in the liver, cholecalciferol is converted to 25-hydroxycholecalciferol which has weak activity. This molecule is then converted in the kideys to 24,25-dihydroxycholecalciferol, which is also weakly active or 1,25-dihydroxycholecalciferol which is the active form of Vitamin D. This active form then goes on to significantly increase the absorption of calcium in the intestines.
Low levels of Vitamin D in children are associated with Ricketts and in adults, low levels lead to osteomalacia (softening of the bones). For years this was pretty much the sum of knowledge about Vitamin D. Researchers now know that the same Vitamin D receptors in the intestine are present in many other organs throughout the body including the heart, the lungs, blood vessels, the prostate, muscles and endocrine glands to name some. These receptors throughout the body have led to research seeking to determine whether Vitamin D has additional roles in human health including with protecting against infections, boosting immunity or quelling inflammation.
Let’s get back to COVID-19 why people think our levels might be important with respect to preventing the illness or protecting against severe disease. For some time there has been evidence that low Vitamin D levels put people at risk for acute respiratory tract infections (ARTI) like ear infections, colds and even pneumonias. Furthermore, studies seem to show that the risk of severe disease and dying has an almost linear relationship with decreasing Vitamin D levels in the population being studied. With the emergence of COVID-19, also an ARTI, researchers started looking at Vitamin D as a possible factor in disease severity. COVID-19 studies show a similar correlation between Vitamin D deficiency and disease severity. In general, it seems the people most at risk for Vitamin D deficiency like those with chronic disease, seniors, and people of color also seem to be at the highest risk for severe COVID-19 disease. A very recent study looked at countries with high prevalence of Vitamin D deficiency and compared them to countries with low prevalence. They found that countries like Sweden, Norway and other Scandinavian countries with low prevalence of Vitamin D deficiency have lower infection rates and fewer deaths. Countries with more Vitamin D deficiency like Spain and Italy have the highest infection and death rates.
So while all of this is compelling on the surface, let’s take a deeper look. The studies on COVID-19 and Vitamin D have all been observational studies. In an observational study, researches simply observe what happened (retrospective) or what happens down the line (prospective) to a group of people and infer from the data they collect. In an observational study, no experiment was applied and tested. It’s just as the name suggests, an observation. This doesn’t make observational studies bad; it’s just important to understand their limitations. The data from observational studies, which are much easier to complete than experimental studies, can be quite compelling and in medicine they often drive interest in the direction of experimental studies. But scientists are hesitant to draw significant conclusions from them because the information shows correlation, not causation. Take for instance this scenario: an eager medical student at a large teaching hospital wants understand the factors that increase likelihood of death during code blue (emergency situation in a hospital involving cardiac or respiratory arrest). Over the course of his ICU rotation he observes the code blue emergencies and records the medications given, amount of oxygen delivered, type of chest compression administered…he observes and records everything he can think of. One day as he’s looking at his data he sees something quite remarkable. One factor stands out for him: the more doctors there are in the room during a code blue, the more likely a patient is to die.
Observational studies provide us with important information but they show correlations, not causations. In fact, you’ve probably heard the saying, “correlation does not equal causation”. As in our example, the number of doctors in the room during a code blue is probably related to (correlates with) the complexity of the patients condition and code event; the sicker the patient or the more difficult the resuscitation, the more doctors are needed. It’s unlikely, we hope, that a higher number of doctors in the room during the code is actually causing the patient to die. So back to our Vitamin D studies. The information obtained in these studies is good but it is observational and by the authors’ own admission, they show correlation not causation. Are the patient’s sicker because they have low Vitamin D levels or are the patients most likely to be sicker (seniors, those with chronic conditions, people of color etc.) people who are also more likely to have low Vitamin D levels. To answer these questions, experimental studies or clinical trials need to be undertaken. In experimental studies we look for the classic double blinded, placebo controlled randomized trial. In other words we want a study in which people are randomized into two groups, one group gets Vitamin D and the other group gets placebo and neither the doctors nor the patients involved in the study know what they’re getting. At the end of the study you look at the data to see which group did better. That gets us on the road to knowing whether Vitamin D is protective against severe COVID-19 disease.
To my knowledge there are no clinical trials on Vitamin D in COVID-19 that have yet reported their results but there are some trials currently underway to assess whether Vitamin D may be helpful in the treatment and/or prevention of severe COVID-19 disease. There’s a study looking at whether a single dose of 25,000 IU of Vitamin D will improve mortality in patients with mild disease. There’s also a study looking at several different doses for patients with more severe disease who are older than 75. Time will tell if Vitamin D plays an important role in COVID-19 but at this point we don’t know, we simply have the correlation.
All that said, we do know that it is not good to have low Vitamin D levels in general. For any person, the goal for all our nutritional indices is to be in the normal range–it’s how we work best. So given that, for patients with COVID-19 it’s reasonable for treating physicians to provide Vitamin D supplementation if levels are low–as would be true with any patient irrespective of COVID-19 status. Whether this helps fight COVID-19 specifically we don’t know yet. We also do not at this point have evidence that people with normal Vitamin D levels should further supplement with Vitamin D in order to protect against COVID-19 disease.
My greater concern with respect to possible links between Vitamin D and COVID-19 is that this questionable connection seems to be being used as an excuse to disregard public health measures that control the spread of SARS-CoV-2. Those who perhaps are already questioning the usefulness of social distancing or stay-at-home orders are suffering from confirmation bias by using the possible link to suggest that these public health interventions are counterproductive or dangerous and should be ignored because they’re keeping people indoors and reducing their sun exposure. At the very least, some are using this data to justify actions known to be dangerous like converging at the beach on a beautiful day. Social media is filling up with claims that if you want to fight the virus, forget this stay-at-home stuff, get out there and get some sun. Go to the beach! Play some sports! The clear implication is that getting Vitamin D is more important than not getting the virus. There is simply no evidence that this is true. If you get the virus you could die or someone you love could die and there’s no evidence your Vitamin D level or sun exposure will save you or your loved one. Short of a vaccine, public health measures like social distancing and stay-at-home are the single most important thing we can do to prevent the spread of this disease to vulnerable populations and subsequently causing preventable deaths. In some ways, outdoor activity and sun exposure is being presented as a false dilemma. Most public health experts (with some exceptions in very densely populated cities) have not restricted people to their homes and have encouraged outdoor activities that adhere to social distancing (no congregating in groups, keep appropriate space especially if exercising) and viral spread control measures (e.g. face masks). If you live in an area where these activities are permitted then by all means please undertake them. Being healthy is always a good thing when it comes to giving human beings a leg up at surviving illness but don’t use this fact to ignore public health measures designed to prevent you from getting COVID-19 in the first place. You really don’t want to get this infection, or at the very least, you don’t want to give it to someone you care about who may not be able to survive it.
One reply on “Vitamin D and COVID-19”
Thanks for this info. There’s so much info/misinfo out there. Were you able to look at the info Paul Marik, MD did on vitamin and Covid-19?
Wife and I just got done discussing what we see is the future of socializing in the community post-corona virus. This thing will probably be around for a while and some form of social distancing is going to be a norm for the next year or two (our opinion). I don’t know if we’ll be eating at a dine in restaurant anytime soon, even when they reopen for that type of service.
Once again, I look forward to your next post.
LikeLiked by 1 person